eISSN 2444-7986
DOI: https://doi.org/10.14201/orl.21305
REVIEW
Cirugía tiroidea de acceso remoto
Jose GRANELL1,2; Kyu Eun LEE3
1 Rey Juan Carlos University Hospital. Mostoles. Madrid. Spain.
2 HLA Moncloa University Hospital. Madrid. Spain.
3 Seoul National University Hospital. Seoul. Korea.
Correspondence: jgranelln@seorl.net
Reception: 20 August 2019
Acceptance: 22 August 2019
Publication: 24 August 2019
Publication of the volume: 1 June 2020
Disclosure: J Granell has a contract with Abex, dealer of the da Vinci robotic surgery system for Spain, Italy and Portugal, for training and proctoring in robotic surgery.
Figures: Authors declare that the images has been obtained with patient´s consent.
Policy of rights and auto-store: it is allowed to auto-store the post-print version (SHERPA/RoMEO)
Licence CC BY-NC-ND. Creative Commons NonComercial 4.0 International Licence
University of Salamanca.
SUMMARY: Introduction and objective: The aim of this paper is to describe the current situation of the so-called remote access thyroid surgery. Although the original motivation for the development of these approaches is cosmetic (to avoid a visible scar on the neck), in practice they have meant a real revolution in the range of technical options for the management of thyroid surgical pathology. Synthesis: In a very short period of time, since year 2000, a number of remote access variants have been tested, finally consolidating four approaches. These are the axillary or transaxillary approach, the bilateral axillo-breast approach, the retroauricular or facelift approach, and the transoral / transvestibular approach. The indications and surgical principles of each of them are described. Conclusions: Remote access thyroidectomy has proved to be safe and effective. There is consensus on its acceptance as an alternative for certain patients. In its undeniable process of expansion, multiple topics of discussion are mixed, such as the debate on the effectiveness of surgical technology.
KEYWORDS: Thyroidectomy, Minimally Invasive Surgical Procedures, Robotic Surgical Procedures.
RESUMEN: Introducción y objetivo: El objetivo de este artículo es describir la situación actual de la denominada cirugía de acceso remoto a la glándula tiroides. Aunque la motivación original para el desarrollo de estos abordajes es cosmética (evitar una cicatriz visible en el cuello), en la práctica han supuesto una auténtica revolución en el abanico de opciones técnicas para el manejo de la patología quirúrgica tiroidea. Síntesis: En un periodo de tiempo muy corto, desde el año 2000, se han testado multitud de variantes de acceso remoto, consolidándose finalmente cuatro abordajes. Estos son el abordaje axilar o transaxilar, el abordaje axilopectoral bilateral, el abordaje retroauricular o de facelift, y el abordaje transoral transvestibular. Se describen las indicaciones y los principios quirúrgicos de cada uno de ellos. Conclusiones: La tiroidectomía de acceso remoto ha demostrado ser segura y eficaz. Existe consenso en su aceptación como alternativa para determinados pacientes. En su innegable proceso de expansión, se mezclan múltiples temas de discusión, como el debate de la eficiencia de la tecnología quirúrgica.
PALABRAS CLAVE: Tiroidectomía; cirugía mínimamente invasiva; cirugía robótica.
Since its description at the end of the 19th century by Theodor Kocher, thyroid gland surgery had not undergone significant technical changes until at the end of the 20th century when the minimally invasive surgical approaches for parathyroidectomy and thyroidectomy began to arise. In 1995, Michael Gagner performed the first endoscopic parathyroidectomy [1] and in 1996 Husher the first endoscopic thyroid lobectomy [2]. The options for applying endoscopic techniques to thyroid and parathyroid surgery were explored for a few years, with the philosophy of minimal incision and minimal dissection. The problems to be solved were diverse. The first and most obvious was that there is no anatomical cavity in the neck, such as the peritoneal cavity, which can be insufflated with gas to maintain the surgical field. In the neck the dissection is performed between fascial layers; to maintain the working space without collapsing, retractors should be used (for example percutaneous Kirshner needles [3]) or CO2 insufflated if the technique allowed for a watertight space. Gas injection in the sub-platismatic plane produced extensive emphysemas in the first experiences (although with the reduction of the pressure of the gas this problem is anecdotal at present). Another problem was the choice of the access points, which progressively moved away from the cervical area, moving from the neck to the infraclavicular area and then to the thorax.
Of these initial experiences, the only one that remains today is Miccoli´s minimally invasive video-assisted thyroidectomy (MIVAT, Minimally Invasive Video-Assisted Thyroidectomy), which found a compromise between minimization of the incision and endoscopic support [4]. However, this technique is only used by some groups of surgeons in various parts of the globe and has the disadvantage that there is still a cervical scar. Therefore, if one of the objectives of this approach is that there are no visible stigmas of surgery, MIVAT is not a good option. Especially when in reality the greater or lesser visibility of the scar does not depend so much on its size as on its final appearance, which is often conditioned by poorly controllable factors.
In year 2000, Yoshifumi Ikeda described the transaxillary thyroidectomy and inaugurated the modern era of remote access to the neck [5]. In the relatively short period of time since then, various options have been tested regarding the number of access points and their location in the pectoral region (already completely avoiding scars in visible areas in the neck), as well as the way of maintaining the surgical field. Although trocars have been used at some time in visible areas of the anterior thoracic wall (for example subxyphoid), with the introduction of the periareolar incision (Ohgami, 2000 [6]) the combinations of axillary and periareolar ports, all of them hidden, have been sufficient. A purely lateral (axillary), latero-medial (axillary and pectoral, such as ABBA, Bilateral Axillo-Breast Approach [7]), or bilateral axillo-pectoral (BABA, Bilateral Axillo-Breast Approach [8]) can be used.
In 2001, Woong Youn Chung introduced the gas-less axillary approach and designed an specific retractor (Chung´s retractor) [9]. In 2007 the same author introduced the robotic instrumentation for this approach [10]. This has been one of the most used approaches to date for remote access thyroidectomy.
Between 2010 (Willhelm and Metzig, through the floor of the mouth [11]) and 2011 (Richmon et al., with robotic instrumentation [12]), transoral thyroidectomy was described. From a series of modifications with the option for the transvestibular route and the new distribution of the incisions, as described by Anuwong, it is consolidated as an emerging technique (TOETVA: TransOral Endoscopic Thyroidectomy - Vestibular Approach) and is probably the approach in more rapid expansion [13].
In 2011, David Terris published the technique for robotic thyroidectomy by a retroauricular approach [14]. Actually, the technique is an expansion of the rhytidectomy approach (facelift) that the same author described in 1994 for parotid gland surgery [15]. This technique has been very well received in various departments of otorhinolaryngology for thyroidectomy and neck dissection.
Outcomes and experience have consolidated four techniques for a remote access to the neck as a result of this process in recent years. Applied to thyroid gland surgery these techniques are axillary or transaxillary thyroidectomy (usually gas-less, and instrumented with robotic or with conventional endoscopic material), thyroidectomy by bilateral axillo-breast approach, BABA (which is a technique with gas, frequently with robotic instrumentation), retroauricular or facelift thyroidectomy (gas-less and usually robotic) and transoral / transvestibular thyroidectomy (more frequently with gas and with conventional endoscopic instruments).
Each has its advantages and limitations. In this article we will describe both the techniques and the indications and limitations of each of them.
TECHNIQUES FOR A REMOTE ACCESS TO THE THYROID GLAND
Remote access thyroid surgery has the particularity that it transforms conventional open thyroidectomy into an endoscopic procedure (instrumented with conventional endoscopic or robotic material). However, the goal of surgery is the same (partial or total removal of the thyroid gland) and even from a technical point of view the surgical steps are very similar. The most obvious difference is that in the remote access there are no visible scars in the cervical region, although the introduction of the technology offers other potential benefits.
To understand the different approaches, we must consider the three options we have to take.
The first decision is whether we are going to use a percutaneous access through an incision or through a direct puncture of the trocars. In this second case the resulting scar will be only that of the trocar puncture, virtually invisible, and we will obtain a watertight cavity that can be insufflated with gas (this is so for BABA and TOETVA). If we make an incision, the function of the trocars will be simply to stabilize the instruments (in case of robotic instrumentation) and we can use more or less depending on the size of the working space (normally four robotic arms in the axillary approach, but only three in the retroauricular). This incision will logically leave a scar, which will be designed to remain hidden (behind the axillary fold or in the retroauricular region), but which will be normally identifiable.
The second decision is the distribution and the number of the access ports (Figure 1). Anatomically with respect to the thyroid region, we can propose a superior or inferior approach, a lateral or a medial approach. The transvestibular and the retroauricular are superior approaches (the first medial and the second lateral), and the BABA and the axillary, inferior (the first medial and the second lateral).
Finally, we must decide if we are going to use robotics or not. The axillary approach and the BABA were instrumented for years with conventional endoscopic material until the introduction of robotics. The retroauricular was directly described as robotic and the transvestibular is performed more frequently with conventional material.
The options are therefore diverse and the choice of one or another technique depends on the experience, the specific indication and other factors. Remote access thyroidectomy is technically challenging. Typically, robotic instrumentation is considered to shorten the learning curve and make the procedure technically easier, although the specific circumstances tend to be more complex because they heavily depend on previous surgical experience.
Let’s see the details of each of the techniques.
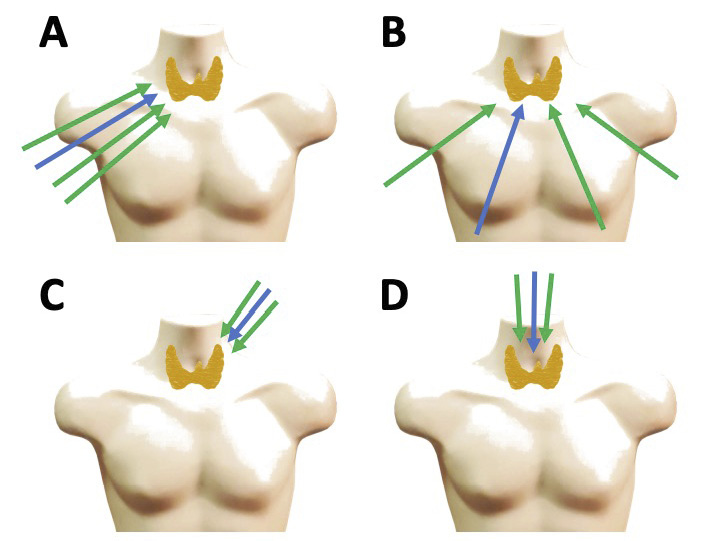
Figure 1. Remote access techniques to the thyroid gland. The blue arrow represents to the endoscope, and the green ones the instruments. A: Axillary or transaxillary approach. It is a lateral and inferior approach that can be performed with gas or gas-less, and with robotic instrumentation (with 4 arms) or non-robotic. B: Bilateral axillo-breast approach. It is a medial and inferior approach with gas, robotic or non-robotic. C: Retroauricular approach. It is a superior and lateral approach, gas-less, with three arms, robotic. D: Transoral / transvestibular approach. It is a superior and medial approach, usually with gas, robotic (with 3 arms) or non-robotic.
The transaxillary approach can be performed through cannula puncture and gas insufflation, although the most common way to apply it is through an incision behind the anterior axillary fold, from which a subcutaneous flap is raised in the pectoral region to access the neck. This gas-less approach requires the use of a retractor to maintain the field. Through this approach the four robotic arms can be introduced, in addition to the auxiliary instruments that are necessary in each surgical step, or the conventional laparoscopic instrumentation, without the need for cannulas.
Transaxillary thyroidectomy in a very standardized technique in which there is extensive clinical experience. The axillary approach allows for thyroidectomy to be carried out in compliance with the most demanding safety standards, including neuromonitoring [16]. Its other great advantage is that it is actually a video-assisted open approach (in a sense similar to MIVAT), which can facilitate the management of certain complications (for example, bleeding) and be a priori more comfortable for some surgeons. It also avoids a very rare, but potentially serious complication associated with the gas that is gas embolism, which can occur, for example, if a jugular vein is accidentally opened [17]. Although morbidity on the shoulder was reported in the initial series associated with the position of hyperextension, these problems have been eliminated by adjusting the patient’s position for the intervention [18].
This approach has two basic problems. The first is that the cosmetic outcome of the scar is usually bad, and although the scar is hidden behind the anterior axillary fold, this may be acceptable in certain cultures (eg Asian), but not so much in others (eg Mediterranean). On the other hand, the approach requires an extensive subcutaneous dissection that actually puts the technique out of the concept of minimal invasion.
Surgically, the approach to the thyroid gland is lateral and inferior, which entails some technical differences with conventional thyroidectomy. The dissection of the flap is subcutaneous in the thorax and sub-plastismatic in the neck, with which the usual anatomical references are exposed: long pre-laryngeal muscles and sternocleidomastoid muscle (ECM). The first important difference is that the separation of the muscles is not done in the midline. According to the access vector, a separation of the clavicular and sternal bellies of the ECM is performed, and the latter is separated superiorly together with the pre-laryngeal (omohyoid, sternothyroid and sternohyoid) of both sides. The midline is therefore kept intact. At this point the thyroid gland is already exposed and it is time to stabilize the retractor and introduce the robotic arms (figure 2).
This approach is usually indicated for hemithyroidectomy, and therefore the access side is the one corresponding to the lobe to be removed. A total thyroidectomy may be performed by a unilateral approach, but lateral dissection of the contralateral lobe (and therefore dissection of the parathyroid glands and recurrent laryngeal nerve) is technically difficult. There is the option of making a bilateral axillary approach, or this can delayed if the anatomopathological analysis of the specimen indicates totalization. However, this approach could be considered to provide excessive morbidity, particularly when there are better alternatives. This problem is shared by lateral approaches. In the case of the retroauricular approach, which has a narrower working corridor, the option of contralateral lobectomy is not even contemplated.
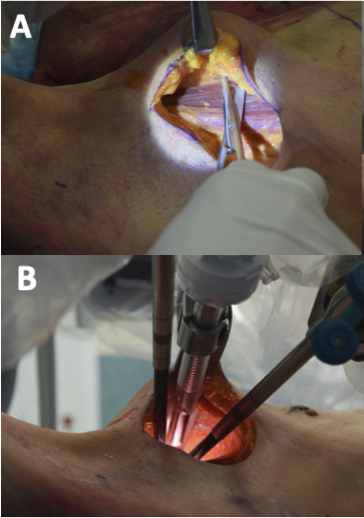
Figure 2. Transaxillary approach (cadaver preparation). A. In clinical conditions, the incision should be traced with the patient standing and the arm at rest to ensure that it is hidden behind the anterior axillary fold. Once the skin and subcutaneous tissue are sectioned, the pectoral muscle is easily identified and its upper surface is followed towards the thyroid region. B. After lifting and stabilizing the skin flap, the robotic arms are introduced. The 30º endoscope is used. The incision allows the introduction of the fourth arm, although attention should be paid to its placement to avoid collisions.
The surgical goals are the same, regardless of the approach. The effective and safe extirpation of the thyroid lobe, preserving the superior and inferior parathyroid glands, and the recurrent and superior laryngeal nerves. The transaxillary thyroidectomy technique was originally described with conventional endoscopic instrumentation, which conditioned some technical handicaps that limited, for example, the performance of contralateral lobectomy [19]. Later, the technique with robotic instrumentation was described, while additional improvements were introduced, such as specific retractors [20]. The instruments are a dissector (eg Maryland dissector), a cutting instrument (usually the harmonic) and a third arm that acts as a retractor (eg. a fenestrated forceps). The surgical steps are the same as in conventional thyroidectomy: ligation of the superior laryngeal pedicle, medial separation of the lobe with identification and preservation of the superior and inferior parathyroid glands and the recurrent laryngeal nerve, completing the lobectomy.
There are extensive series that support the surgical and oncological safety of robotic transaxillary thyroidectomy [21].
Thyroidectomy by bilateral axillo-breast approach
The bilateral axillo-breast approach (BABA) is a medial and inferior approach, with gas, which provides a surgical field very similar to that of conventional thyroidectomy. Unlike the axillary approach, the patient is placed without shoulder extension, in a more natural position. Some cervical extension is required, as in conventional thyroid surgery, and a small posterior rotation of the shoulders. An additional advantage of the BABA, and in general of the gas-less access, is that they do not require separators or retractors to maintain the surgical field, since it is the gas insufflation itself that performs this function.
BABA thyroidectomy is a very standardized technique, which with minor modifications is performed similarly in all centers [22]. Like the axillary approach, it was initially described with conventional endoscopic instrumentation [23]. However, robotic instrumentation provides the advantage of a high-definition three-dimensional image that facilitates the identification of structures, and above all a dexterity in the manipulation that compensates for the limitations of the work in a confined field.
The anatomical references, entry ports and trajectories of the endoscope and instruments are outlined on the skin (Figure 3). The subcutaneous area is injected with saline in the area of the flap. Then the skin incisions are made and blunt dissection of the tunnels is done following the corresponding trajectories. The first tunnel will be that of the endoscope, which will be introduced through the ipsilateral breast port. Once the first trocar is introduced, CO2 insufflation is done, at a low pressure (8 mmHg with a maximum flow of 20 L / mn). A 30º endoscope facing down is used. Under endoscopic control, the raising of the flap will be completed until an adequate working space is obtained (figure 4). Regarding the instrumentation, it will be the same as for the transaxillary approach, using the four arms with similar purposes although with much lower risk of collisions thanks to the much more favourable access trajectories. Alternatively to the harmonic, we can use as a cutting instrument the monopolar hook, which can speed up the work in certain steps, and will also act as a probe for the stimulator of the neuromonitor [24]. One of the basic rules is that the surgery be as bloodless as possible, since the control of bleeding is substantially hindered in a confined field and is one of the most important conversion risks.
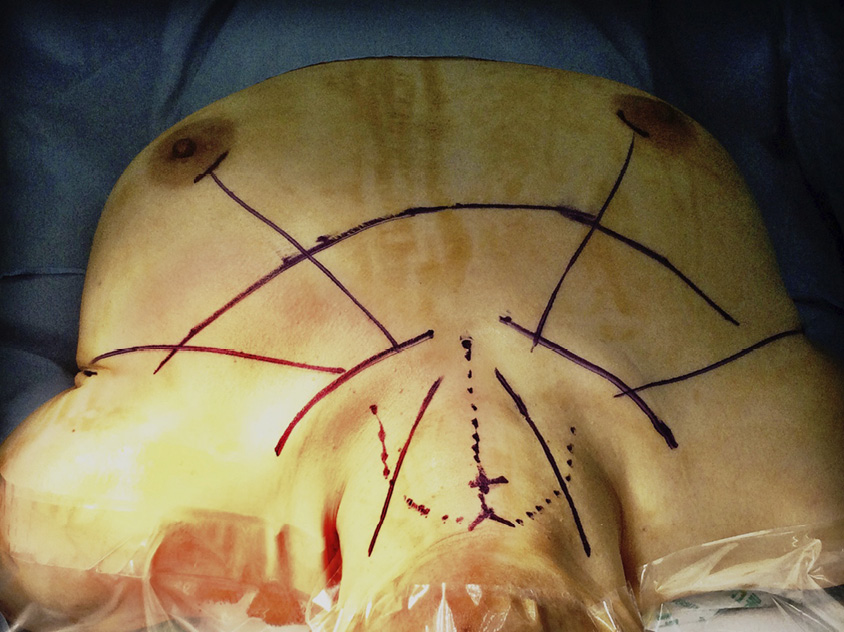
Figure 3. Anatomical references for BABA. View from the patient’s head. It is appropriate to outline them in the cervical-pectoral area once the field is draped. The first mark is the superior notch of the thyroid cartilage (“V”) and the midline of the cricoid cartilage (“+”), in addition to the anterior border of the sternocleidomastoid muscle bilaterally and the superior border of the clavicles. We mark the midline from the notch to the yugulum, and the approximate area of the cervical flap that we need to raise. The access ports are arched incisions in the superomedial border of both areolas, and two linear incisions in skin folds in both axillas. The trajectory of the instruments goes from the access ports towards the midline of the cricoid. We will also need some skin dissection below the clavicles so that the instrument arms have enough freedom of movement.

Figure 4. Surgical field for BABA thyroidectomy. The midline and anterior border of the right ECM have been marked. Note that the perspective is very similar to what we have in a conventional thyroidectomy and that gas insufflation provides a very comfortable working field.
Due to the type of instrumentation, the thyroidectomy technique differs in some steps from the open conventional technique. Once the midline prelaryngeal musculature is separated, the isthmus of the thyroid gland is divided to facilitate medial traction. The most important modification is that the dissection of the gland is performed from inferior to superior, ultimately sectioning the superior pedicle. Laterally, the recurrent laryngeal nerve and the superior and inferior parathyroid glands must be identified and preserved. Likewise, before sectioning the upper pedicle, the upper laryngeal nerve must be identified. The same procedure is repeated on the other side if a total thyroidectomy is to be performed. If central neck nodes dissection is required, it can be performed with the same field.
Also, extensive series support the surgical and oncological safety of BABA thyroidectomy [25]. The technology provides resources that can potentially improve functional outcomes, regardless of the better visualization and more careful dissection, such as the identification and intraoperative confirmation of the viability of the parathyroid glands with indocyanine green [26].
On the other hand, although technically difficult, the BABA is an excellent access for lateral neck lymph node dissection [27], even if it is to be bilateral [28].
Facelift approach for thyroidectomy
The rhytidectomy incision is designed to work on the face and cervical region through camouflaged incision lines in the pre and retroauricular areas, and in the scalp area of the neck. It allows to work directly in the parotid region and the high laterocervical area. There is extensive experience in surgery on the parotid gland through this incision, which is currently a standard [29] (Figure 5). The lower and anterior extension of the skin flap allows to expose the entire neck, including the thyroid region. A suitable retractor is needed to keep the flap elevated and a video-assisted technique to work in the most distal areas.
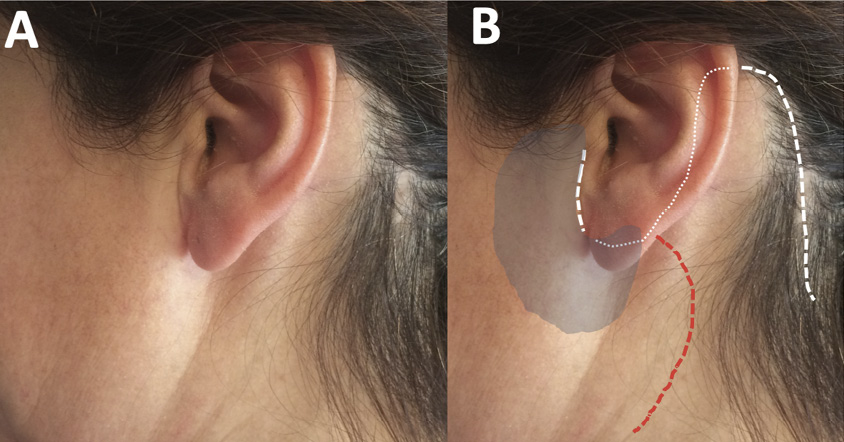
Figure 5. Facelift incision. A. Cosmetic outcome of a parotidectomy. B. Unlike the Blair incision that has a cervical part (red line), the rhytidectomy or facelift (white line) incision has all of its parts camouflaged. It provides access to both the parotid (shaded) region, and the upper portion of the laterocervical area directly. For the robotic approach to the thyroid gland, the preauricular part is not required.
Retroauricular thyroidectomy shares with the axillary approach that both are open and lateral approaches; the latter inferior, and the first superior. The retroauricular approach requires a smaller detachment of the skin, but provides a narrower working corridor, which limits, for example, contralateral lobectomy. However, if surgery of the lateral neck is to be performed, part of the procedure can be done with a conventional open technique, introducing the robotic instrumentation just for the most distal areas.
The technique of thyroid lobectomy by facelift approach is a standard technique that was originally described with robotic instrumentation [30]. The patient is placed supine, without cervical extension, with the neck lateralized 30º. A modified facelift incision is used, without the preauricular part of the incision. The incision and the initial dissection of the flap are done in a standard way. In the upper areas, caution should be taken not to injure the great auricular nerve. Subsequently, the ECM muscle serves as a reference to continue the subplastismatic dissection of the flap inferior and anterior, with the aid of progressively longer retractors and long monopolar tips. Next we will find the omohyoid muscle and more medially the sternohyoid and the sternothyroid. Separating this muscles from lateral to medial we will expose the upper pole of the thyroid gland. They are held in this position with a retractor and then the robotic arms are introduced. The 30º endoscope (down) and two instruments, a dissector (Maryland) and a cutting instrument (harmonic) are used.
Since access to the thyroid gland is superior, the first surgical step will be the ligation of the superior pole that is subsequently pulled inferiorly and medially to identify in the lateral area first the upper parathyroid gland and the recurrent laryngeal nerve, and then the inferior parathyroid. Once these structures are identified, the tissue medial to them is sectioned, including the ligament of Berry, and finally the inferior thyroid vein. After checking the hemostasis, the skin incision is sutured; normally drains are not used.
The retroauricular approach has had particular acceptance in the otolaryngology departments, possibly because all the work is done in a very familiar surgical territory and does not require the use of CO2. This acceptance includes more generally than for other approaches, centers outside the Asia-Pacific area [31]. In addition to thyroidectomy, the retroauricular approach is suitable for other interventions on the lateral neck such as submaxilectomy [32] or lymph node dissection [33]. The retroauricular approach is experimenting a development for cervical surgery other than thyroidectomy in the West, which had had no other approaches [34].
As mentioned above, transvestibular thyroidectomy is probably the fastest expanding technique. Although it has been described with different types of instrumentation, including the new single-port robotic system [35], probably its most common application is with conventional laparoscopic instrumentation. Its great advantage is its feasibility with adjusted costs (due to conventional instrumentation), in addition to the obvious absolute absence of visible scars. Its limitations are, on one hand the technical difficulty and on the other a restricted working corridor that limits procedures to thyroidectomy and dissection of the central compartment.
Although it can be performed as an open procedure with the aid of retractors, it is usually performed with gas. It may have access limitations depending on the anatomical configuration of each patient. Typical complications in the initial cases were related to the lesion of the mental nerves. Modifying the incisions has solved this problem.
Currently, transvestibular thyroidectomy with conventional endoscopic instruments (TOETVA) is a standardized technique [36]. The patient is placed supine with a slight cervical extension and the surgical field is draped in the usual way, exposing the mouth which is washed with an antiseptic solution. The incisions are made in the mucosa of the lower lip. A medial incision is required for the endoscope, which will have a horizontal trajectory above the labial frenulum, and two lateral ones for the instruments, with a vertical direction (Figure 6). The central incision is deepened with monopolar cautery through the mental muscle to the tip of the chin. A saline solution is then injected through the incision to hydrodissect the cervical area. Next with a dissector (eg Kelly) the plane between the platysma muscle and the prelaringeal muscles is dissected. Once this plane is defined, the dissection is extended with a tunneler and the trocar of the endoscope is inserted. CO2 is insufflated with a pressure of 6 mmHg at low flow (15 L / mn). The surgical field is vertically between the thyroid cartilage and the sternal yugulum, and laterally to both ECM. The instrumentation is done with laparoscopic surgery material: monopolar hook, dissectors (Maryland) and harmonic, and visualization with a 30º endoscope (figure 7). The prelaryngeal muscles are divided in the midline and dissected from the thyroid lobe. The pyramidal lobe of the thyroid gland is dissected first and the isthmus is sectioned. Subsequently Joll’s avascular space is identified to separate the upper pole and identify the upper pedicle, which is sectioned with the harmonic. The thyroid lobe is then separated medially to expose the tracheoesophageal groove and to identify the recurrent laryngeal nerve, which will be preserved along with both parathyroid glands (upper and lower). Finally, the Berry ligament is sectioned and the piece is removed in an endobag. If a total thyroidectomy is to be performed, the procedure is repeated on the other side. The prelaryngeal musculature is sutured in the midline and incisions are closed with an absorbable suture. The patient must wear a compressive dressing for the first 24 hours (analogous to that used for lifting).
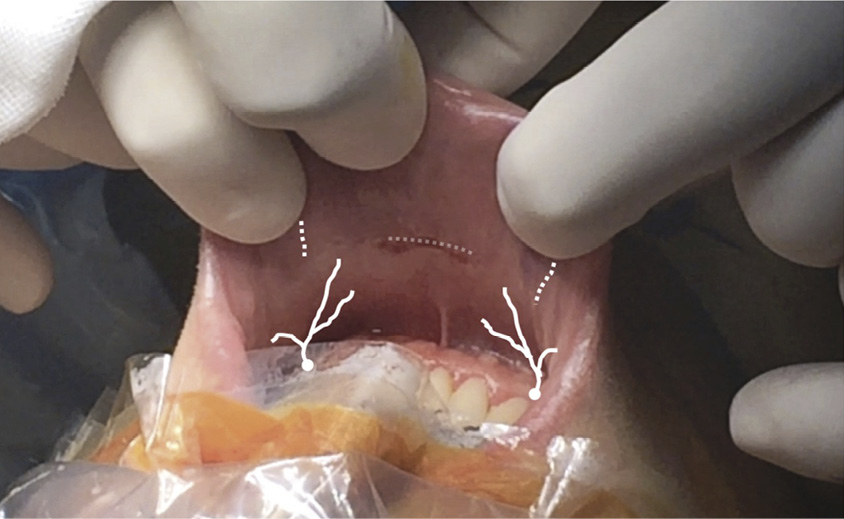
Figure 6. Incisions for TOETVA in the mucosa of the lower lip. Medial incision of 10 mm, horizontal, above the labial frenulum and two lateral incisions of 5 mm, vertical, displaced superiorly and laterally to avoid injury to the branches of the mental nerves that emerge from the jaw at the level of the canines.
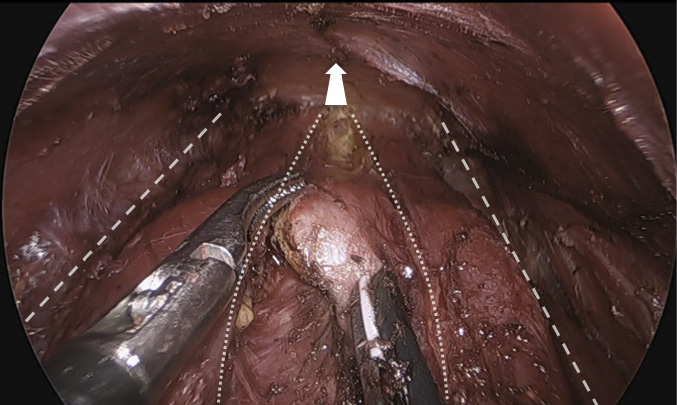
Figure 7. Surgical field of the transvestibular approach to the thyroid gland. The arrow points in the lower direction (sternal yugulum). The medial edges of the ECM (striped lines) and the prelaryngeal musculature, already separated in the midline (dotted lines) have been marked. The surgeon is instrumenting with a Maryland dissector on his left hand and a harmonic on the right, and is sectioning the isthmus of the thyroid gland. In the upper part of the image you can see the inner side of the skin flap, maintained by the gas.
Although one of the initial concerns regarding this approach was the risk of infection, since access is made through a contaminated area (the vestibule of the mouth), the fact is that there are no communications of postoperative infections in the published series, already very numerous. However, perioperative antibiotic coverage is used.
Transvestibular thyroidectomy is safe and effective. Since its initial development stadardization was seeked, and there are international groups of experts devoted to it [37].
All the techniques presented have proven to be safe and effective and with all of them there is significant experience. The choice of one or the other has historically been conditioned by the place and the center where they have been developed and probably also by a surgeon training bias depending on his or her origin in otolaryngology - head and neck surgery, or general surgery / endocrine surgery. It is often difficult to make comparisons between them. However, we can make some generalizations (Table 1).
Table 1. Characteristics of remote access options for thyroid surgery (adapted from a suggestion of Pro. Kyung Tae). Indicative quantitative assessment (plus / less from 1 to 4 “+”; “-“ if not possible. In red the best option for each feature).
|
Approach |
Axilar |
Axilopectoral Bilateral |
Retroauricular (facelift) |
Transoral / transvestibular |
|
Feature |
||||
|
Invasiveness |
++++ |
+++ |
+++ |
++ |
|
Working space |
+++ |
++++ |
+++ |
++ |
|
Total thyroidectomy |
+ / - |
++++ |
- |
++++ |
|
Central dissection |
+++ |
+++ |
+++ |
+++ |
|
Lateral dissection |
++++ |
++++ |
++++ |
- |
|
Postoperative pain |
++ |
++ |
++ |
++ |
|
Cosmetic outcome |
++ |
++++ |
+++ |
++++ |
|
Complications |
+ |
+ |
+ |
+ |
Gas-less techniques generally require a wider dissection of tissues that can potentially generate more morbidity. Of these, axillary thyroidectomy is the oldest and has been one of the topics for criticism on robotic thyroidectomy [38]. These criticisms had to do with the justification of the approach itself and with the costs associated with robotic instrumentation. The experience accumulated in later years has served to overcome this point of view in the debate, although it is likely that the axillary approach will be abandoned, preserving an historical value. The retroauricular is probably not the best approach for thyroidectomy. However, as we have said, it has potential indications for many surgical diseases of the lateral neck.
Among the medial approaches with gas, we have already pointed out the advantages of the non-robotic transvestibular approach (TOETVA) and the reasons for its current expansion. Its limitations are related on the one hand with the learning curve and on the other with the indications, not only those depending on the thyroid disease itself, but also for its limitation to the central neck compartment. The robotic BABA is also a technically difficult approach, but it does not have many of the limitations of TOETVA.
In year 2016, the American Thyroid Association (ATA) published a positioning paper on remote access thyroid surgery [39]. Although it pointed out a series of restrictions, in practice it opened a door. The ATA document was written with much more limited series than we have now and did not even consider the transvestibular approach.
On the road traveled so far, progress has been made in the indications and some limitations have been overcome: in the maximum size of the nodules or of the thyroid gland itself, in the approach of benign or malignant pathology, in the indication or not in the Graves disease thyroidectomy, etc. It is probably reasonable that at least part of this path is traveled again in the departments in which the techniques are introduced [40].
The debate that remains is how much investment in technology do we need to progress in the remote access. The need for some of these technologies is indisputable, such as advanced cutting and coagulation systems, or neuromonitoring systems. And the robotics? There is no doubt that current robotic surgery is the most advanced and refined form of endoscopic surgery we have. And so is that an important part of the future development of surgery will go this way. The development of the techniques stimulates the creation of new technology and viceversa. There is no doubt that technological development expands what is feasible, and that the expansion of endoscopic surgery and minimally invasive approaches has been and is closely linked to technological development. Even so, as surgeons we must maintain a critical spirit and check which procedures bring benefit to our patients and which are more efficient.
Remote access thyroidectomy currently includes four stablished approaches: transaxillary thyroidectomy, bilateral axillo-breast approach, retroauricular and transoral / transvestibular. All of them have proven to be safe and effective techniques for the treatment of surgical pathology of the thyroid gland, including thyroid cancer. Each one has its indications and its limitations.
The original justification for these approaches is primarily cosmetic (to avoid a visible scar on the neck) and therefore, in addition to meeting criteria for indication, patients must have a high degree of motivation to opt for these approaches.
The introduction of different technologies entails certain modifications in the surgical technique whose potential benefit, in addition to the cosmetic, must be proved.
J Granell wants to acknowledge the Spanish Society of Otolaryngology – Head and Neck Surgery for the support in his trainning in remote access surgery in Seoul. Also, to the centers in which this trainning was done, particularly to the department of surgery of Seoul National University, but also to Bundang (Prof. June-Young Choi and Hyeong-Won Yu), Chung Ang Hospital (Prof. Kyung-Ho Kang and Ra-Yeong Song), Hanyan Hospital (Prof. Kyung Tae), and to Prof. Se-Heon Kim from Yonsei University.
1. Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg.1996;83:875.
2. Hüscher CS, Chiodini S, Napolitano C, Recher A. Endoscopic right thyroid lobectomy. Surg Endosc.1997;11:877.
3. Shimizu K, Akira S, Tanaka S. Video-assisted neck surgery: endoscopic resection of benign thyroid tumor aiming at scarless surgery on the neck. J Surg Oncol. 1998;69:178-80.
4. Miccoli P, Berti P, Raffaelli M, Conte M, Materazzi G, Galleri D. Minimally invasive video-assisted thyroidectomy. Am J Surg. 2001;181:567-70.
5. Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M. Endoscopic neck surgery by the axillary approach. J Am Coll Surg 2000;191:336-340
6. Ohgami M, Ishii S, Arisawa Y, Ohmori T, Noga K, Furukawa T, Kitajima M. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech. 2000;10:1-4.
7. Shimazu K, Shiba E, Tamaki Y, Takiguchi S, Taniguchi E, Ohashi S, Noguchi S. Endoscopic thyroid surgery through the axillo-bilateral-breast approach. Surg Laparosc Endosc Percutan Tech. 2003;13:196-201.
8. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, Oh SK, Youn YK. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007;31:601-6.
9. Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS, Nam KH, Chang HS, Chung WY, Park CS. Gasless endoscopic thyroidectomy using trans-axillary approach; surgical outcome of 581 patients. Endocr J. 2009;56:361-9.
10. Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS. Excellence in robotic thyroid surgery: a comparative study of robot-assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg. 2011;253:1060-6.
11. Wilhelm T, Metzig A. Video. Endoscopic minimally invasive thyroidectomy: first clinical experience. Surg Endosc. 2010;24:1757-8.
12. Richmon JD, Pattani KM, Benhidjeb T, Tufano RP. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head Neck. 2011;33:330-3.
13. Anuwong A, Ketwong K, Jitpratoom P, Sasanakietkul T, Duh QY. Safety and Outcomes of the Transoral Endoscopic Thyroidectomy Vestibular Approach. JAMA Surg. 2018;153:21-7.
14. Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: II. Clinical feasibility and safety. Laryngoscope. 2011; 121:1636-41.
15. Terris DJ, Tuffo KM, Fee WE Jr. Modified facelift incision for parotidectomy. J Laryngol Otol. 1994;108:574-8.
16. Dionigi G, Kim HY, Wu CW, Lavazza M, Materazzi G, Lombardi CP, Anuwong A, Tufano RP. Neuromonitoring in endoscopic and robotic thyroidectomy. Updates Surg. 2017;69:171-9.
17. Kim KN, Lee DW, Kim JY, Han KH, Tae K. Carbon dioxide embolism during transoral robotic thyroidectomy: A case report. Head Neck. 2018;40:E25-E28.
18. Alkan U, Zarchi O, Rabinovics N, Nachalon Y, Feinmesser R, Bachar G. The cause of brachial plexopathy in robot-assisted transaxillary thyroidectomy. A neurophysiological investigation. Laryngoscope. 2016;126:2187-93.
19. Ikeda Y. Totally endoscopic thyroidectomy: axillary approach. En D.J. Terris, M.C. Singer (eds.), Minimally Invasive and Robotic Thyroid and Parathyroid Surgery. Cap 7. Pp. 49-53. Springer Science+Business Media New York 2014
20. Lee S, Chung WY. Robot-Assited transaxillary thyroidectomy. En D.J. Terris, M.C. Singer (eds.), Minimally Invasive and Robotic Thyroid and Parathyroid Surgery. Cap 9. Pp. 67-76. Springer Science+Business Media New York 2014
21. Chai YJ, Lee KE, Youn YK. Can robotic thyroidectomy be performed safely in thyroid carcinoma patients? Endocrinol Metab (Seoul). 2014;29:226-32.
22. Robotic thyroidectomy: Bilateral Axillo-Breast Approach. En Youn YK, Lee KE, Choi JI, Color Atlas of Thyroid Surgery, Cap. 4, pp. 83- 126. Springer-Verlag Berlin Heidelberg 2014
23. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, Oh SK, Youn YK. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007;31:601-6.
24. Sung ES, Lee JC, Kim SH, Shin SC, Jung DW, Lee BJ. Development of an Attachable Endoscopic Nerve Stimulator for Intraoperative Neuromonitoring during Endoscopic or Robotic Thyroidectomy. Otolaryngol Head Neck Surg. 2018;158:465-8.
25. Lee KE, Kim E, Koo do H, Choi JY, Kim KH, Youn YK. Robotic thyroidectomy by bilateral axillo-breast approach: review of 1,026 cases and surgical completeness. Surg Endosc.2013;27:2955-62.
26. Yu HW, Chung JW, Yi JW, Song RY, Lee JH, Kwon H, Kim SJ, Chai YJ, Choi JY, Lee KE. Intraoperative localization of the parathyroid glands with indocyanine green and Firefly(R) technology during BABA robotic thyroidectomy. Surg Endosc. 2017;31:3020-7.
27. Yu HW, Chai YJ, Kim SJ, Choi JY, Lee KE. Robotic-assisted modified radical neck dissection using a bilateral axillo-breast approach (robotic BABA MRND) for papillary thyroid carcinoma with lateral lymph node metastasis. Surg Endosc. 2018; 32:2322-7.
28. Song RY, Sohn HJ, Paek SH, Kang KH. The First Report of Robotic Bilateral Modified Radical Neck Dissection Through the Bilateral Axillo-breast Approach for Papillary Thyroid Carcinoma With Bilateral Lateral Neck Metastasis. Surg Laparosc Endosc Percutan Tech. 2018 Oct 31. doi: 10.1097/SLE.0000000000000590. [Epub ahead of print]
29. Grover N, D’Souza A. Facelift approach for parotidectomy: an evolving aesthetic technique. Otolaryngol Head Neck Surg. 2013;148:548-56.
30. Singer MC. Robotic Facelift Thyroidectomy. En D.J. Terris, M.C. Singer (eds.), Minimally Invasive and Robotic Thyroid and Parathyroid Surgery. Cap 10. Pp. 77-84. Springer Science+Business Media New York 2014.
31. Duke WS, Holsinger FC, Kandil E, Richmon JD, Singer MC, Terris DJ Remote Access Robotic Facelift Thyroidectomy: A Multi-institutional Experience. World J Surg. 2017;41:116-21.
32. Singh RP, Sung ES, Song CM, Ji YB, Tae K. Robot-assisted excision of the submandibular gland by a postauricular facelift approach: comparison with the conventional transcervical approach. Br J Oral Maxillofac Surg. 2017;55:1030-4.
33. Ji YB, Song CM, Bang HS, Park HJ, Lee JY, Tae K. Functional and cosmetic outcomes of robot-assisted neck dissection by a postauricular facelift approach for head and neck cancer. Oral Oncol. 2017;70:51-7.
34. Albergotti WG, Byrd JK, Nance M, Choi EC, Koh YW, Kim S, Duvvuri U. Robot-Assisted Neck Dissection Through a Modified Facelift Incision. Ann Otol Rhinol Laryngol. 2016;125:123-9.
35. Park YM, Kim DH, Moon YM, Lim JY, Choi EC, Kim SH, Holsinger FC, Koh YW. Gasless transoral robotic thyroidectomy using the DaVinci SP system: Feasibility, safety, and operative technique. Oral Oncol. 2019;95:136-42.
36. Anuwong A, Sasanakietkul T, Jitpratoom P, Ketwong K, Kim HY, Dionigi G, Richmon JD. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): indications, techniques and results. Surg Endosc. 2018;32:456-65.
37. Dionigi G, Tufano RP, Russell J, Kim HY, Piantanida E, Anuwong A. Transoral thyroidectomy: advantages and limitations. J Endocrinol Invest. 2017;40:1259-63.
38. Inabnet WB 3rd. Robotic thyroidectomy: must we drive a luxury sedan to arrive at our destination safely? Thyroid. 2012; 22: 988-90.
39. Berber E, Bernet V, Fahey TJ 3rd, Kebebew E, Shaha A, Stack BC Jr, Stang M, Steward DL, Terris DJ; American Thyroid Association Surgical Affairs Committee. American Thyroid Association Statement on Remote-Access Thyroid Surgery. Thyroid. 2016;26:331-7.
40. Razavi CR, Tufano RP, Russell JO. Starting a Transoral Thyroid and Parathyroid Surgery Program. Curr Otorhinolaryngol Rep. 2019;7:204-8.